 A study from Bristol University, UK exploring the impact of poor sleep on brain development.
A study from Bristol University, UK exploring the impact of poor sleep on brain development.
Researchers conclude that poor sleep may be a cause, not a result, of symptoms of “schizophrenia”, or indeed many other problems.
The original article in Neuron, is very technical – see end of this post. For an explanation in human language see the piece by Caroline Clancy from Eureka Alert.
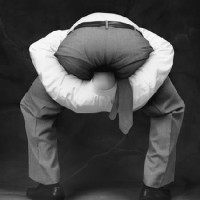
So, yet again scientists are working on demonstrating what we already know, in this case: go long enough without sleep and you’ll start to experience a different “reality”.
As the saying goes don’t try this at home, especially without a designated driver, but if you want a very personal, deeply immersive learning experience of what it’s like to experience visions, unusual thoughts or hearing voices, without doing anything else [and there are plenty of extra things you can do to accelerate the process] all you need do is simply go without sleep for long enough.
Public release date: 14-Nov-2012
Caroline Clancy
University of Bristol
Could poor sleep contribute to symptoms of schizophrenia?
Neuroscientists studying the link between poor sleep and schizophrenia have found that irregular sleep patterns and desynchronised brain activity during sleep could trigger some of the disease’s symptoms. The findings, published in the journal Neuron, suggest that these prolonged disturbances might be a cause and not just a consequence of the disorder’s debilitating effects.
The possible link between poor sleep and schizophrenia prompted the research team, led by scientists from the University of Bristol, the Lilly Centre for Cognitive Neuroscience and funded by the Medical Research Council (MRC), to explore the impact of irregular sleep patterns on the brain by recording electrical brain activity in multiple brain regions during sleep.
For many people, sleep deprivation can affect mood, concentration and stress levels. In extreme cases, prolonged sleep deprivation can induce hallucinations, memory loss and confusion all of which are also symptoms associated with schizophrenia.
Dr Ullrich Bartsch, one of the study’s researchers, said: “Sleep disturbances are well-documented in the disease, though often regarded as side effects and poorly understood in terms of their potential to actually trigger its symptoms.”
Using a rat model of the disease, the team’s recordings showed desynchronisation of the waves of activity which normally travel from the front to the back of the brain during deep sleep. In particular the information flow between the hippocampus — involved in memory formation, and the frontal cortex — involved in decision-making, appeared to be disrupted. The team’s findings reported distinct irregular sleep patterns very similar to those observed in schizophrenia patients.
Dr Matt Jones, the lead researcher from the University’s School of Physiology and Pharmacology, added: “Decoupling of brain regions involved in memory formation and decision-making during wakefulness are already implicated in schizophrenia, but decoupling during sleep provides a new mechanistic explanation for the cognitive deficits observed in both the animal model and patients: sleep disturbances might be a cause, not just a consequence of schizophrenia. In fact, abnormal sleep patterns may trigger abnormal brain activity in a range of conditions.”
Cognitive deficits — reduced short term memory and attention span, are typically resistant to medication in patients. The findings from this study provide new angles for neurocognitive therapy in schizophrenia and related psychiatric diseases.
Paper
The study, entitled ‘Decoupling of Sleep-Dependent Cortical and Hippocampal Interactions in a Neurodevelopmental Model of Schizophrenia’ by Keith G. Phillips(1, 2, 3), Ullrich Bartsch(2, 3), Andrew P. McCarthy(1), Dale M. Edgar (1), Mark D. Tricklebank(1), Keith A. Wafford(1), Matt W. Jones(1,2), was published in the journal Neuron on 8 November 2012.
1. Lilly Centre for Cognitive Neuroscience, Eli Lilly and Company
2. School of Physiology and Pharmacology, MRC Centre for Synaptic Plasticity, University of Bristol
3. These authors contributed equally to this work
The research was funded by the Lilly Centre for Cognitive Neurosciences, the pharmaceutical company Eli Lilly & Co, and the Medical Research Council.
original paper
Decoupling of Sleep-Dependent Cortical and Hippocampal Interactions in a Neurodevelopmental Model of Schizophrenia
Keith G. Phillips, Ullrich Bartsch, Andrew P. McCarthy, Dale M. Edgar, Mark D. Tricklebank, Keith A. Wafford, Matt W. Jones
http://www.sciencedirect.com/science/article/pii/S0896627312008513


































































































Not that surprising, is it?! When I have a sleepless night, I definitely get ‘discombobulated’, and who knows what discombobulation could become, given half a chance…. 🙂
LikeLike
I wonder does …discombulated
come before or after ….wibbly, wobbly and wibbly wobbly??
LikeLike
Before….. as far as I can tell in this state 🙂
LikeLike